Category: Uncategorized

One Survivor’s AI Breakthrough Predicts Cancer Years Ahead
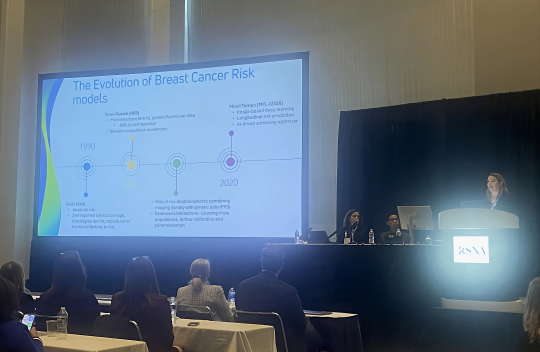
AI Decoded focusses on one of the most urgent, tangible uses of artificial intelligence: health care — we speak to Dr Regina Barzilay, an MIT professor who is building machine-learning AI models to predict disease. She herself was diagnosed with breast cancer in 2014, and has used that experience and knowledge to target her research towards prevention — the AI model she and her team built, named MIRAI, is now able to detect a patient’s risk of developing breast cancer within five years. Are we on the brink of a revolution in treating cancer for everyone? Find out on AI Decoded... Joining presenter Christian Fraser is AI Decoded co-host Stephanie Hare and the BBC's AI correspondent Marc Cieslak Learn more
Meet the newest Forbes 30 under 30
Gabriele Corso was a computer science PhD student at MIT's Computer Science and Artificial Intelligence Laboratory (CSAIL), where his research focused on the intersection of machine learning and molecular biology. His cofounder Saro Passaro was also a research scientist at MIT and previously worked at Meta. The two have trained AI models for predicting biomolecular structures and how molecules interact within the body, which could eventually help with drug discovery. Used by thousands of global organizations and downloaded more than 1M times, these open source models are the basis for Boltz, a company Corso and Passaro cofounded with Jeremy Wohlwend to improve therapeutic design using AI. Learn more
3 lessons from the biotech revolution that can shape U.S. innovation today
Nobel-Prize-winning scientist Phil Sharp could have easily never come to discover RNA splicing, which launched the biotechnology revolution, in 1977. In many ways, the odds were stacked against him: He grew up on a farm in rural Kentucky, he struggled with dyslexia, and neither of his parents had attended college.Still, his parents encouraged him to go to college, and he saved money for tuition from raising cattle and selling tobacco. Sharp’s grit, combined with an innovation ecosystem in the U.S. that invested in science, created the environment that led to a triumph not just for Sharp, but also America’s ability to innovate, according to Youseph Yazdi, assistant professor and executive director of the Center for Bioengineering Innovation & Design at Johns Hopkins University.
At a recent screening of the documentary Cracking the Code: Phil Sharp and the Biotech Revolution, Yazdi and the film’s director, Bill Haney, discussed the key lessons from this breakthrough that can inform the way the U.S. approaches innovation in a new era of great power competition. Learn more
What will be the first AI-designed drug? These disease-fighting antibodies are top contenders
Antibodies — immune proteins that recognize foreign molecules, such as those made by pathogens, with exquisite specificity — have been a challenge for AI to design. AI models such as AlphaFold have struggled to predict the shape of flexible loop regions of antibodies, which they use to recognize their targets.But new tools developed in the past year — including an updated version of AlphaFold — have proved better at modelling these flexible regions, says Gabriele Corso, a machine-learning scientist at the Massachusetts Institute of Technology in Cambridge. Progress in antibody design has followed.
In October, Corso and his colleagues described the BoltzGen model in a preprint, showing that it can adroitly design ‘nanobodies’ — small, simple antibodies resembling molecules made by sharks and camels — against proteins implicated in cancer, viral and bacterial infections and other diseases. In most cases, the researchers identified antibodies with strong target binding after expressing just 15 of the most-promising designs in cells and testing them in laboratory experiments. However, the molecules were not tested in disease models. Learn more
MIT scientists debut a generative AI model that could create molecules addressing hard-to-treat diseases
More than 300 people across academia and industry spilled into an auditorium to attend a BoltzGen seminar on Thursday, Oct. 30, hosted by the Abdul Latif Jameel Clinic for Machine Learning in Health (MIT Jameel Clinic). Headlining the event was MIT PhD student and BoltzGen’s first author Hannes Stärk, who had announced BoltzGen just a few days prior. Learn more