Personalizing the future of breast cancer screening
88 Hospitals, 22 Countries
Breast cancer is the #1 most common cancer in women worldwide. Half of breast cancers develop in women who have no identifiable risk factors other than gender and age.
We believe that every person has the right to know their risk of developing cancer. Mirai is a deep learning model that produces a personalized risk score up to 5 years in advance just by analyzing a patient’s mammogram, ensuring that cancer can be detected early.
Mirai has been validated extensively on mammograms from patients all over the world. Thanks to the support of Wellcome Trust, we have been able to expand the deployment of Mirai to include hospitals serving under-resourced regions. This validation process is key to ensuring that Mirai maintains high performance and that it can be safely used on real patients.
Try Mirai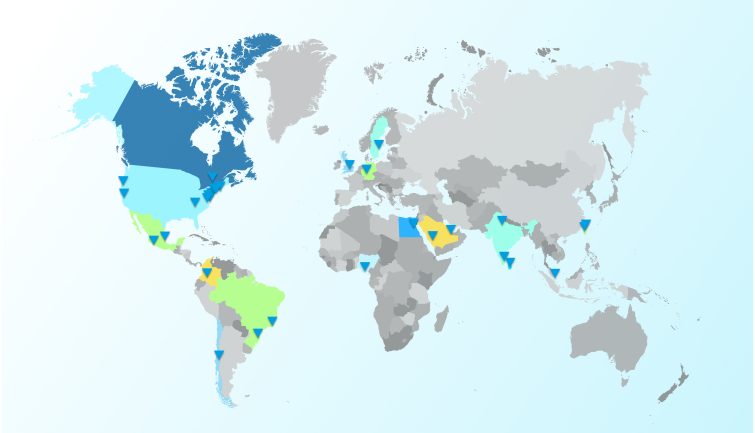
Collaborate with us
Hospitals around the world have installed Mirai, with some publishing independent research on Mirai.
We welcome hospitals to join our Hospital Network.

How does Mirai work?
In Japanese, “mirai” (未来) means future.
Mirai produces a risk score that helps the clinician determine if a patient requires additional screening if the patient is high-risk, or if the patient can avoid unnecessary screening if they are low-risk.

The team behind Mirai
MIT Jameel Clinic AI faculty lead Regina Barzilay decided to build Mirai after completing her breast cancer treatment in 2016, when she learned there were no clinically-available AI models that assess breast cancer risk.
Joined by then-student Adam Yala and Mass General Brigham radiologists, Barzilay led the team to develop the technology behind Mirai.
The scale and computational power needed for bold ideas to work is not possible without the support of grants, foundations, and donors. Your support would enable MIT Jameel Clinic to make a better, healthier future for all.
Give NowU.S. Core Collaborators





International Core Collaborators








Regional Leads



Alumni

NEWS